Minimally invasive surgery and Metabolic care. Technical approaches
February 17, 2014
A. Parisi
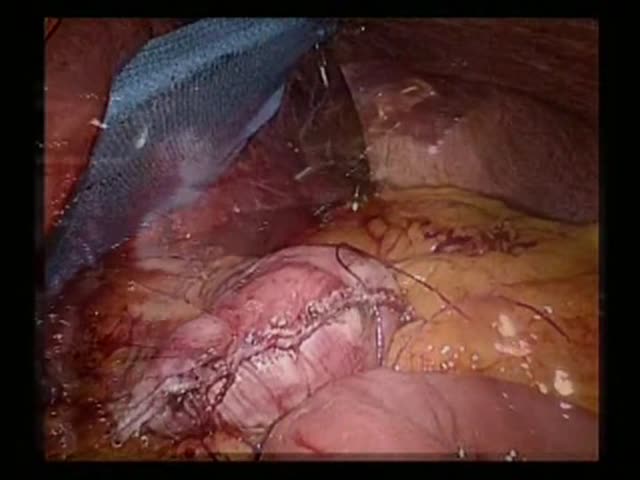
Actually, the role of bariatric surgery is achieving great attention for the treatment of metabolic diseases and particularly type 2 diabetes mellitus (T2DM) in combination with different degrees of obesity. According to the current American Diabetes Association (ADA) and the National Heart, Lung, and Blood Institute (NHLBI) guidelines, bariatric surgery is a treatment option to be offered to patients who have clinically severe obesity (BMI> 40) or a BMI> 35 and serious comorbid conditions. Studies report results on T2DM relative to follow-up in the short and medium term and show rapid resolution or improvement of diabetes in 65-85% of patients. Minimally invasive approach has gained consensus not only among physicians but also among patients because of its efficacy and no significant post-operative morbidity. In our Institute we perform routinely bariatric intervention with the aid of laparoscopic technology and “Da Vinci Si” robotic surgical system. The video shows the performance of a gastric bypass with mixed minimally invasive techniques. In particular we highlight the features of both laparoscopic and robotic approach in the execution of a gastric pouch and the subsequent gastro-jejunal anastomosis. The first surgical time is performed in laparoscopic surgery. A small (20ml) gastric pouch is created of approximately 10cm along the lesser curve and the proximal stomach is transected delimiting the inferior border of the pouch with a linear stapler. After adeguate preparation of the left diaphragmatic pillar, it’s cut the lateral bord of the pouch up to gastroesophageal junction, with a linear stapler and on the guide of a transoral 36F tube. The second time takes place with the aid of the “Da Vinci” robotic surgical system. In particular the video shows a side-to-side one-row gastro-jejunal anastomosis performed with running PDS 2-0 suture. The procedure shown in the video was executed in a 50-year-old women, with uncontrolled T2DM and BMI = 41,8 kg/m2, at the Department of Digestive Surgery and Liver Unit, St. Maria Hospital, Terni, Italy. The preoperative HbA1C value was 7.6% reduced to 5.8% after 18 months from surgery without the use of medications. BMI after the same period decreased to 32.6 kg/m2. Surgery demonstrates efficacy to improve metabolic diseases and large studies should investigate the real role, hormonal modifications and the correct time to perform it. A team specializing in minimally invasive techniques and a multidisciplinary centre for obesity, as in our Institute, are needed for a successful treatment in patients with metabolic disorders.