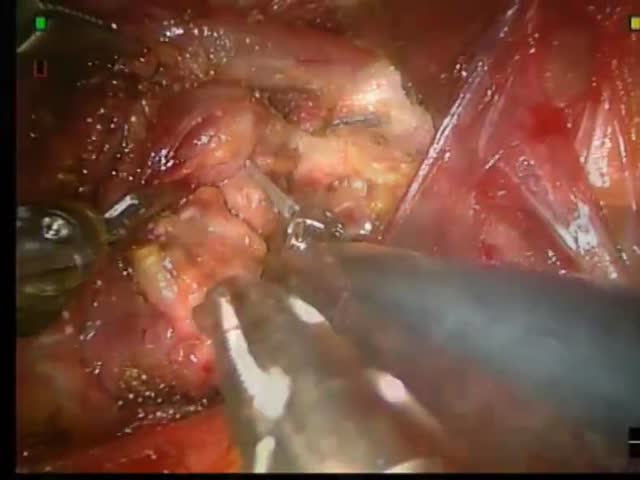
Chicago 2009 Video – Robotic Transaxillary Completition thyroidectomy for sospicius thyroid cancer with parathyroid reimplantation
January 16, 2010
G. Caravaglios
Robot assisted thyroidectomy has been recently becoming more popular and successfully used in United States and Korea. Technical limitations and precise indications still have to be defined. The presence of scar and adhesions due to previous lobectomy could increase the difficulty of the procedure. The potential benefits of the minimally invasive approach in this context are not only the avoidance of the neck scar (already present), but the accuracy and precision connected to improved vision, magnification and microdissection abilities.
The present video is showing the case of a 61 years old female, who previously underwent a right hemithyroidectomy 15 years ago for a benign thyroid nodule. The patient presented a 3 cm new nodule in the left residual lobe. A fine needle aspiration cytology revealed a TIR2 risk for cancer. After proper consent obtained the planned offered procedure was a robotassisted transaxillary completion thyroidectomy (left lobectomy). A 5 cm longitudinal incision was done along the anterior pillar of the left axylla and a 7 mm incision, for the fourth robotic arm, in the presternal area. A subcutaneous “tunnel” , above the major pectoralis muscle fascia, was prepared from the axillary incision to reach the left lateral-cervical region.
A retractor was used to lift the subcutaneous tunnel. Access to the left thyroid lobe was achieved through the two heads of the sterno-cleido-mastoid muscle. The initial dissection was done with a careful use of the monopolar hook, more effective then the harmonic due to the presence of scar tissue. The ultrasound dissector was used to transect the vascular pedicles, and in proximity of the laryngeal nerve, very well defined. The superior left parathyroid gland looked ischaemic and decision was taken to reimplant it. A muscular pocket was created in the pre-thyroid muscle for the reimplantation. The operative time was 90 minutes. The patient was discharged two days after surgery in good condition. A transient, asymptomatic hypocalcemia occurred for two days. No laryngeal deficit was evident. Final pathological diagnosis was Hashimoto thyroiditis.
Results
The operative time was 90 minutes. The patient was discharged two days after surgery in good condition. A transient,
asymptomatic hypocalcemia occurred for two days. No laryngeal deficit was evident. Final pathological diagnosis was
Hashimoto thyroiditis
Conclusions
The robotic technique provides not only cosmetic benefits (no scar in the neck), but also enhances visualization, precision and dexterity decreasing the risk of specific morbidity. Furthermore, the postero-lateral approach to the thyroid region allows the avoidance of the most sclerotic anterior planes encased in the old scar.